Health Problems of Low Birth Weight Babies on Family and Society
- Enquiry
- Open Admission
- Published:
The impact of preterm nascency <37 weeks on parents and families: a cantankerous-exclusive study in the 2 years after discharge from the neonatal intensive intendance unit
Health and Quality of Life Outcomes volume 15, Commodity number:38 (2017) Cite this commodity
Abstract
Background
Piddling is known nearly the quality of life of parents and families of preterm infants after belch from the neonatal intensive care unit of measurement (NICU). Our aims were (i) to describe the impact of preterm nativity on parents and families and (two) and to identify potentially modifiable determinants of parent and family unit touch.
Methods
We surveyed 196 parents of preterm infants <24 months corrected age in three specialty clinics (82% response charge per unit). Main outcomes were: (ane) the Impact on Family unit Scale total score; and (2) the Infant Toddler Quality of Life parent emotion and (3) time limitations scores. Potentially modifiable factors were use of community-based services, financial burdens, and health-related social bug. We estimated associations of potentially modifiable factors with outcomes, adjusting for socio-demographic and infant characteristics using linear regression.
Results
Median (inter-quartile range) infant gestational age was 28 (26–31) weeks. Higher Affect on Family scores (indicating worse effects on family functioning) were associated with taking ≥3 unpaid hours/week off from work, increased debt, financial worry, dangerous home environment and social isolation. Lower parent emotion scores (indicating greater bear upon on the parent) were likewise associated with social isolation and unpaid time off from work. Lower parent fourth dimension limitations scores were associated with social isolation, unpaid time off from work, financial worry, and an dangerous home environment. In contrast, higher parent fourth dimension limitations scores (indicating less impact) were associated with enrollment in early on intervention and Medicaid.
Conclusions
Interventions to reduce social isolation, lessen financial burden, amend home prophylactic, and increase enrollment in early intervention and Medicaid all accept the potential to lessen the impact of preterm birth on parents and families.
Background
In the United States, nearly 500,000 infants, or eleven.7% of all live births, are born preterm (<37 weeks' gestation) each year [1, ii]. Preterm nascency and the sometimes associated prolonged newborn hospitalization are not bad family stressors, and can lead to subsequent family dysfunction [3–5].
All preterm infants are at risk for re-hospitalization, as well equally medical and neurodevelopmental complications, fifty-fifty moderate to tardily preterm infants (built-in at 32 to <37 weeks' gestation) [6]. A particularly challenged sub-group is very low nascency weight (VLBW) infants or those born < 1500 g. More than than 90% of VLBW infants are discharged dwelling from the neonatal intensive intendance unit (NICU). The brunt of continued health and developmental problems faced by these infants is substantial [7–9]. For example, compared with normal birth weight children, VLBW children face a 2–three fold greater risk for visual and hearing damage, speech communication delays and attention disorders [10, 11]; may have poor feeding and growth, respiratory complications, and face up neurocognitive difficulties [12–16].
Given these ongoing problems and risks, families of preterm children oft must manage numerous medical and developmental needs above and beyond what is required for a healthy total term infant, for months or even years after the neonatal discharge. For instance, during the first yr of life, VLBW infants are prone to re-hospitalization and crave increased outpatient care [17–19]. Parents must transport their child for medical appointments and therapies, communicate with the child's pediatrician and other healthcare providers, and are frequently responsible for daily tasks, such as administering medications and monitoring chronic conditions.
The intensity of care and loftier level of vigilance required by families to run across the needs of their preterm child makes it likely that having a preterm child adversely affects the quality of life of the parents and the family unit overall. The 2006 Institute of Medicine's (IOM) report on Preterm Nascency: Causes, Consequences and Prevention stressed the importance of assessing aspects of family and parent quality of life and stress beyond maternal psychological well-beingness [twenty–22]. A better agreement of the impact of preterm birth on parent and family quality of life, every bit well as modifiable factors that predispose parents and families to greater or bottom impact would inform community-based and other structured assistance programs designed to lessen the impact.
Our main research question was, "Are modifiable characteristics (such as the use of community based and public assistance programs, fiscal burden, and health related social issues) associated with the impact of preterm nativity on parents and families after NICU belch?" The Anderson and Aday health utilization model [23, 24] provides a useful framework for addressing our research question because it uniquely captures the constructs of admission, need, and quality of life. As presented in Fig. ane, nosotros conceptualized potentially modifiable characteristics that influence parent and family unit bear on as: (ane) utilise of community based developmental services and public help programs; (2) financial brunt; (iii) health related social problems. We also specified predisposing characteristics (including socio-demographics and infant wellness characteristics) related both to modifiable characteristics and to outcomes that could human action as confounders.
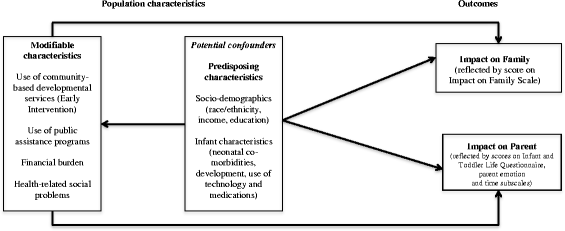
Conceptual Model. Adapted from Phillips [74]
Our specific aims were (1) to describe the touch of preterm birth on parents and families and (2) and to identify potentially modifiable determinants of parent and family bear on. Specific variables of interest based on previous literature, were employ of community-based resource, financial brunt and wellness-related social problems [25].
Methods
Study pattern and participants
This was a cantankerous-sectional study. Nosotros enrolled one parent (mother or male parent) of preterm (<37 weeks gestation) infants attending three outpatient clinics at a large third children's infirmary. One dispensary provides multidisciplinary medical and neurodevelopmental follow-upwardly for infants with gestational historic period <32 completed weeks or birth weight <1500 m discharged from 1 of three large, academic NICU'south and affiliated community-based Level Ii nurseries, and for more mature or heavier preterm infants with severe medical weather condition and/or social gamble factors (101 participants enrolled). The 2d clinic provides pediatric pulmonary care for infants with lung disease that originates in the newborn menses, predominantly bronchopulmonary dysplasia (57 participants enrolled). The 3rd clinic provides follow-up care for infants who have suffered neurologic injury during the fetal or newborn menstruation (38 participants enrolled). While some patients were seen at more than than one clinic, they were only enrolled once in the study.
We included parents of preterm infants who were up to 24 months corrected age (historic period from term equivalent). Parents must accept been able to answer questions in English or Spanish. If the infant was a multiple, only i response was collected from the family. Study staff provided eligible families with a letter describing the written report. Consent was obtained when the parent agreed to complete the questionnaire, which was administered on a laptop (with privacy screens) in the clinic waiting room or examination room. Participants were provided a minor incentive to complete the survey.
The Boston Children'south Infirmary and Children's Infirmary Los Angeles human subjects committees approved the written report protocol. Approximately 75% of preterm infants are referred to high-risk infant follow up programs. [iii] In this study, of the 239 eligible participants from October, 2011 to June, 2012, 196 completed the questionnaire (82% response rate). The questionnaire is available equally Additional file ane.
Measurements
Measurements of primary outcomes, modifiable characteristics and potential confounders (predisposing characteristics) are summarized in Additional file 2: Table S1.
Impact on family
The Bear upon on Family (IOF) [26–28] measures the global touch on of pediatric disability on the family and has been validated on samples of children with chronic health conditions, including preterm birth [25]. The IOF total score is derived from a 27-item questionnaire. For each item, parents indicate the extent to which they agree with a statement regarding the negative touch on of the child on the family. Anchors for a 4-bespeak Likert scale were: strongly agree; agree; disagree; and strongly disagree. Examples of IOF items are: "The illness is causing financial bug for the family" and "Our family gives upwards things because of illness." IOF subscales include financial impact (8 points), disruption of planning (20 points), caretaker burden (12 points), and familial burden (sixteen points) for full possible score of 56 points. The total negative bear upon score served as our summary measure of family burden (college scores indicate greater family unit brunt).
In a previous written report, internal consistency was loftier for the overall IOF Scale (Cronbach alphas for total impact, 0.83 to 0.89), but lower for financial (0.68 to 0.79) and coping (0.46 to .52) items [26]. High total scores on the IOF are associated with maternal psychiatric symptoms, poor child wellness, poor child adjustment, increased child hospitalizations, lower maternal education, and maternal receipt of public assist [27–29], providing show for construct validity.
Impact on parent
The Baby Toddler Quality of Life Questionnaire™ (ITQOL) was developed in 1994 for use in children from 2 months to v years of age as a "contour mensurate" for health status and health-related quality of life. ITQOL adopts as its conceptual framework the Globe Health Organization's definition of health as a state of consummate physical, mental and social well-being and not just the absence of affliction [30]. It has been used both in randomized clinical trials [31] and observational studies, and is accustomed favorably for its ease of use and understandability [32].
In this study, we used the Family unit Burden scales of the ITQOL, which encompass 2 parent-focused concept subscales, affect-emotion and touch-time, due to caring for their infant or toddler [30, 32, 33]. The parent impact-emotion domain consists of seven items in which the parent is asked to rate how much anxiety or worry each of the child characteristics described in the items has caused during the by 4 weeks (i.e., feeding/sleeping/eating habits; physical health, emotional well existence, learning abilities, ability to interact with others; behavior and temperament). The parent touch on-time domain consists of seven items in which the parents is asked to charge per unit how much of his/her time was express for personal needs because of the issues with the child'due south personal needs during the past 4 weeks. Internal consistency for the ITQOL parent-impact emotion and parent-impact time scales has been reported in three different populations, a Dutch full general population sample (0.61, 0.64) [34], a functional abdominal pain sample (0.72, 0.73) [35] and a burn injury sample (0.79, 0.84) [30, 36].
Raw subscale scores are converted to standardized scores on a 0–100 continuum [37–forty]. For each scale, college scores point less emotional touch and fewer time limitations on the parent (in other words, higher scores represent more favorable outcomes).
Potentially modifiable characteristics
Employ of community-based resource
Participants were asked yes/no questions about the use of community-based developmental resources (such every bit early intervention programs), use of social services such as food assistance programs, Supplemental Diet Aid Program and the Women, Infant, Children's program as well as free energy assistance/disability programs such the Low Income Home Energy Assist Plan, Transitional Aid to Families with Dependent Children, and receipt of Supplemental Security Income (SSI).
Fiscal Burden
In addition to questions nigh employment for the participating parent and his/her partner, we asked 6 yes/no questions from the 2007 Democracy Fund Biennial Health Insurance Survey [41–44] regarding unexpected costs, increased bills, increased out-of-pocket expenses and financial worry.
Health-related social problems
HelpSteps.com is a survey designed to identify health-related social issues. Development of HelpSteps involved literature review and fundamental informant interviews with wellness and social services experts, yielding an initial list of 25 social domains. Of those, the five near relevant domains were identified using a modified Delphi technique: (i) access to wellness care, (2) housing, (3) food security (4) income security and (five) intimate partner violence [45–48]. Most questions near these domains were adapted from previous surveys (e.g. National Wellness Interview Survey [49], the American Housing Survey [50], the Philadelphia Survey of Work and Family [51] and the Childhood Community Hunger Identification Project [52]), while a few newly written items were likewise incorporated into the terminal HelpSteps survey. In terms of content validity, the domains covered in HealthSteps are well-recognized equally being closely tied to health outcomes and costs [53]. HelpSteps is highly constructive in identifying problems that can be addressed by referral to advisable social services [46, 47] and a qualitative study revealed that over 2/3 of participants found the HealthSteps questions to be highly relevant to their own issues [48].
Predisposing characteristics (potential confounders)
Infant wellness and development
Nosotros obtained information from the medical record regarding commitment and complications during the neonatal hospitalization. We asked parents questions nigh their infant's health status since belch including the number of emergency department visits, monthly clinic appointments, and hospitalizations, immunizations, dependence on engineering, and administration of prescription medications.
To assess infant evolution, we used the Motor and Social Development (MSD) scale [54], which was developed by the National Center for Health Statistics to measure motor, social and cognitive development of young children. Of 48 items derived from standard measures of child evolution, including the Bayley Scales, Gesell Scale, and Denver Developmental Screening Exam, parents complete xv age-specific items, which inquire most specific developmental milestones such every bit laughing out loud, pulling to stand, and maxim recognizable words [55]. We selected the MSD because it is brief and allows for scoring based on a big, national sample [56] with a normative mean of 100 and standard divergence 15, similar to other developmental tests. Higher scores betoken meliorate development. In a previous written report of sometime preterm infants, nosotros showed that the MSD has practiced internal consistency (Cronbach alpha 0.65-0.88) and is modestly correlated with Bayley Scales of Infant and Toddler Devleopment, 3rd edition, a gold standard professionally administered neurodevelopmental test [56]. Another written report reported that infants with lower gestational age at nascence take lower scores on the MSD [54]. Although the MSD includes a cognitive, motor, and social subscales, the degree to which it is sensitive to language/communication delays is unknown, which is a potential limitation.
Statistical analysis
Our principal outcomes were: (1) affect on family unit full score; (2) impact on parent score determined by the concept of emotion; and (3) bear on on parent score determined past the concept of limitation of time. Potentially modifiable determinants included the use of community-based resources, financial burden, and wellness-related social problems. Potential confounders (predisposing characteristics) were socio-demographics and infant pre-disposing and post-belch characteristics.
In bivariate analyses, we compared issue scores across categories of predisposing characteristics (potential confounders) and potentially modifiable determinants. We calculated p-values using non-parametric tests (Wilcoxon Rank Sum or Kruskal Wallis). To place potentially modifiable determinants independent of confounders on our principal outcomes, we created parsimonious multivariable models, adjusting for variables of a priori interest and for other characteristics found to exist significant at p <0.1. We also examined each model using variance inflation factors (VIF) and did not notice meaning collinearity (VIF ≤ ii for all models).
We used SAS version 9.4 (SAS Establish Inc., Cary, NC) for analyses.
Results
Participant characteristics and outcomes
Predisposing characteristics of report participants and outcome measures are shown in Table 1. A bulk of participants were white, non-Hispanic (67%). 52% reported an annual household income of ≥ $80,000 and 68% of mothers had attended at least some college. The median (IQR) gestational age of infants at birth was 28 weeks (26–31). The median (interquartile range, IQR) chronologic historic period of infants at the time of study participation was 10.4 months (seven.5-17.2).
Unadjusted associations of predisposing characteristics (potential confounders) with outcomes
As shown in Tabular array 1, amidst pre-disposing characteristics, the use of medical technology, receipt of at least 1 prescription medication daily, one or more readmission or emergency department visit after neonatal discharge, and 2 or more than clinic appointments per calendar month were all associated with greater bear on on family, parents, or both. Additionally, having an infant with a low developmental score (MSD < 85) was associated with greater impact on the family unit and parent emotion. Fathers who completed the survey had higher bear on scores than mothers on the parent-focused domains of emotion and time limitations. Of notation when we performed an boosted sensitivity analysis past running our multivariate models for mothers just, we found our multivariate model estimates were like in magnitude and management as the total models that included fathers.
Potentially modifiable characteristics and unadjusted associations with outcomes
Table ii shows that apply of public housing and public assistance program were associated with greater impact on family unit. Compensation for time taken off from piece of work was associated with a lower parent emotional score (less parental impact) while use of social services, public housing, enrollment in Medicaid and an unsafe home environment were associated with a higher IOF score (greater family bear upon). Markers of financial burden (including unpaid time off work, increased out-of-pocket expenses, bills, debt and financial worry) and social isolation were associated with both greater family and parental bear on.
Adjusted associations of potentially modifiable characteristics with outcomes
Table 3 shows associations of potentially modifiable characteristics with the total IOF Scale scores, adjusting for potential confounders. Taking time off from work without pay, increased bills, financial worry, an dangerous dwelling house environment, and social isolation were all associated with higher full IOF scores, indicating greater impact. Similarly, Table iv shows adapted associations of potentially modifiable characteristics with impact on Parent Emotion and Time Limitation scores. Taking time off from work without pay and social isolation were associated with lower scores on both of these scales, indicating greater bear upon. Fiscal worry was associated with greater touch on on parent time limitation, equally was an unsafe home environment. In contrast, enrollment in early on intervention and Medicaid programs were associated with higher parent time limitation scores, indicating less parental impact.
Give-and-take
In this study, we described the impact of preterm nascence on parents and families in the first 2 years afterwards neonatal discharge. Our results support our conceptual model, which posits modifiable factors that are associated with the impact of preterm nascency on parents and families, independent of infant wellness and socio-demographic characteristics. Nosotros identified several potentially modifiable factors that were associated with both higher and lower impact. In particular, social isolation, financial burdens such as taking unpaid time off from work, increased bills and financial worry, and an unsafe dwelling house environment were all associated with higher impact on at least i of our principal outcomes. In dissimilarity, enrollment in early intervention and Medicaid and utilize of public housing were associated with less parent bear on.
Predisposing characteristics such as infant co-morbidities afflicted both impact on family scores and parental scores. Infant development affected parental scores for increased feet and emotion. Our findings were consequent with previous studies that the impact was greater amid families whose preterm children demonstrated either a functional handicap or low developmental quotient [22, 25, 57–59]. We besides found that the utilise of prescription medications and durable medical equipment affected both parental touch scores and impact on family scores, which was consistent with other publications [20, 60]. Specifically, the use of medications and medical equipment may contribute to the substantial out-of-pocket expenditures that families may incur [61, 62]. Equally pressure mounts to reduce hospital length of stay and readmission rates, and every bit we move more than complex care into the community, high out-of-pocket costs is an important factor that tin contribute to parental and family strain.
Several studies take shown that preterm birth and an infant's hospitalization can adversely touch on the finances of families after the birth of a preterm or VLBW infant [20, 60–63]. However, little is known about a more than modifiable determinant such as the specifics of financial burden faced by families, or nearly the bear upon of financial burden on parent quality of life. In our study, we constitute that a lack of bounty for fourth dimension off work was associated with both family and parent-time impact scores. As well, increased bills due to hospitalization and increased financial worry were associated with greater bear on. Complementing our findings, 2 studies take reported the out-of-pocket costs incurred by families of preterm infants for outpatient services, medications, likewise every bit indirect costs like lost productivity are significant especially during the kickoff year after discharge [60, 64]. Specifically, Hodek et al. cited that co-payments for outpatient ancillary services and medications increased parental out-of-pocket expenses. Moreover, lost wages for missing work days may increase income losses [60]. Overall, by highlighting the specific aspects of financial burden most closely associated with parent and family bear on, such as lack of compensation and increased bills, our results may inform targeted financial support programs for families of preterm infants after discharge. Moreover, our findings back up that while annual income was not associated with impact on family, parental perspective on fiscal burden was, which should likewise be considered when caring for these families.
Another modifiable determinant are wellness related social problems. These are economic and social problems that tin can affect health such every bit nutrient insecurity and substandard housing [45]. Prior studies have demonstrated the touch of substandard housing on child wellness such every bit increased communicable diseases and injury [65]. All the same, we found that an unsafe dwelling house environment was associated with agin parent-time affect and impact on the family. Timely receipt of public housing has been associated with improved health in other medical condtions [66]. Addressing housing concerns for families of preterm infants through existing public housing programs is a feasible approach to reducing the parental and family affect.
Another health related social problem that was associated with greater parental and family unit impact was social isolation. Other studies that have examined families of premature infants have found that "alienation" [67] and social isolation may take profound bear upon on parental emotion [68]. Jackson et al. described the image of the process of acclimatization of caring for a premature baby as breach, responsibility, confidence and familiarity, and that alienation may be protracted in this population [67]. Intervention strategies that have improved parental emotions oftentimes include education-behavioral models. For case, the Creating Opportunities for Parent Empowerment (COPE) program created by Melnyk, et al. was associated with reduced parental impact during transition abode from the NICU [69, 70]. It is possible that programs like that one benefit families past reducing social isolation in months to years after discharge.
Another modifiable determinant is enrollment in a customs-based developmental program similar "Early Intervention (EI)," was associated with less impact on parental limitation of time. A recent meta-analysis suggests that customs-based developmental programs had beneficial pooled effects on maternal feet, depressive symptoms, and self-efficacy [71]. Moreover, other studies have suggested that these programs can also empower families because of the collaborative procedure that EI offers; in turn, they take a deeper understanding of their child's developmental needs [72].
Similarly to early intervention, we constitute that receipt of Medicaid was associated with lower impact scores on limitations on time. Other studies take demonstrated families who were registered with Medicaid showed improved "parent role confidence" and "parent-baby interaction" than those with private insurance [69]. While this event was unexpected, information technology has been speculated that parents with a higher socioeconomic status and individual insurance may have higher expectations for themselves [69] and therefore may perceive an increased parental touch on on their time versus those who use Medicaid. Overall, our results suggest that greater participation in public assist programs may lessen familial and parental brunt for this patient population.
A strength of our study was our high response rate (82%). Characteristics of the infants were very similar to other follow-up programs [25]. However, we studied families of infants presenting for follow-upwardly intendance rather than the underlying population of families of infants receiving neonatal intensive care, potentially limiting generalizability. Moreover, we did sample both mothers and fathers, which may affect how some of our results are interpreted and parent gender may influence some of the measures including financial burden and social isolation [73]. Also, our study was cross-sectional making us unable to establish causation. While nosotros adjusted for a number of potential confounders, similar all observational studies, ours is subject to residual confounding. While we did non have a full term cohort command in comparing [25], nor data on those not enrolled, our aim was to elicit the feel of parents and families of preterm infants, as well as relationships with modifiable characteristics specific to this population.
Conclusions
In summary, we identified several predictors of increased family and parent impact in families of preterm infants. Of particular interest were the potentially modifiable factors including social isolation and fiscal burden, which were associated with greater touch, and use of community-based developmental services, public housing, and Medicaid which were associated with less bear upon. Our results propose that interventions to target these factors, for instance social and financial support programs, and efforts to increase enrollment in community-based developmental services and public health insurance programs, might lessen the bear upon of preterm nascency on parents and families.
Abbreviations
- IOF:
-
Impact on family total score
- ITQOL:
-
Babe toddler quality of life
- MSD:
-
Motor and social evolution
- NICU:
-
Neonatal intensive care unit
- PFB:
-
Perceived fiscal burden
References
-
Hamilton Exist, Hoyert DL, Martin JA, Strobino DM, Guyer B. Almanac summary of vital statistics: 2010–2011. Pediatrics. 2013;131:548–58.
-
Wang CJ, McGlynn EA, Brook RH, et al. Quality-of-care indicators for the neurodevelopmental follow-upwards of very depression nascence weight children: results of an expert panel procedure. Pediatrics. 2006;117:2080–92.
-
Newborn AAoPCotFa. Hospital discharge of the high-gamble neonate. Pediatrics. 2008;122:1119–26.
-
Garfield L, Holditch-Davis D, Carter CS, et al. Risk factors for postpartum depressive symptoms in low-income women with very low-birth-weight infants. Adv Neonatal Intendance. 2015;15:E3–8.
-
Howe TH, Sheu CF, Wang TN, Hsu YW. Parenting stress in families with very low nativity weight preterm infants in early infancy. Res Dev Disabil. 2014;35:1748–56.
-
Thygesen SK, Olsen M, Ostergaard JR, Sorensen HT. Respiratory distress syndrome in moderately belatedly and late preterm infants and risk of cerebral palsy: a population-based cohort written report. BMJ Open up. 2016;six:e011643.
-
Vohr BR, Wright LL, Dusick AM, et al. Neurodevelopmental and functional outcomes of extremely low nativity weight infants in the National Constitute of Kid Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics. 2000;105:1216–26.
-
Hack K, Taylor HG, Drotar D, et al. Chronic weather condition, functional limitations, and special wellness care needs of schoolhouse-aged children born with extremely low-nativity-weight in the 1990s. JAMA. 2005;294:318–25.
-
Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–nine.
-
McCormick MC, Richardson DK. Premature infants abound upward. North Engl J Med. 2002;346:197–8.
-
Cheung PY, Barrington KJ, Finer NN, Robertson CM. Early childhood neurodevelopment in very low birth weight infants with predischarge apnea. Pediatr Pulmonol. 1999;27:xiv–20.
-
de Kieviet JF, Piek JP, Aarnoudse-Moens CS, Oosterlaan J. Motor development in very preterm and very low-nascency-weight children from birth to adolescence: a meta-assay. JAMA. 2009;302:2235–42.
-
Aarnoudse-Moens CS, Smidts DP, Oosterlaan J, Duivenvoorden HJ, Weisglas-Kuperus N. Executive function in very preterm children at early schoolhouse age. J Abnorm Child Psychol. 2009;37:981–93.
-
Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-assay of neurobehavioral outcomes in very preterm and/or very low nascency weight children. Pediatrics. 2009;124:717–28.
-
de Kieviet JF, Zoetebier L, van Elburg RM, Vermeulen RJ, Oosterlaan J. Brain evolution of very preterm and very low-birthweight children in childhood and adolescence: a meta-analysis. Dev Med Child Neurol. 2012;54:313–23.
-
Burnett Ac, Scratch SE, Lee KJ, et al. Executive Role in Adolescents Born <1000 one thousand or <28 Weeks: A Prospective Accomplice Report. Pediatrics 2015.
-
Donohue PK. Wellness-related quality of life of preterm children and their caregivers. Ment Retard Dev Disabil Res Rev. 2002;8:293–seven.
-
Escobar GJ, Joffe S, Gardner MN, Armstrong MA, Folck BF, Carpenter DM. Rehospitalization in the first 2 weeks after discharge from the neonatal intensive care unit. Pediatrics. 1999;104:e2.
-
Joffe Southward, Escobar GJ, Blackness SB, Armstrong MA, Lieu TA. Rehospitalization for respiratory syncytial virus among premature infants. Pediatrics. 1999;104:894–ix.
-
Als H, Behrman R, Checchia P, et al. Preemie abandonment? Multidisciplinary experts consider how to best meet preemies needs at "preterm infants: a collaborative arroyo to specialized care" roundtable. Modernistic Healthc. 2007;37:17–24.
-
Behrman RaB, Equally. 2007. Washington D.C.: National Academies Printing (US); Preterm Nascency: Causes, Consequences, and Prevention.
-
Cronin CM, Shapiro CR, Casiro OG, Cheang MS. The impact of very low-birth-weight infants on the family unit is long lasting. A matched control study. Curvation Pediatr Adolesc Med. 1995;149:151–8.
-
Aday LA, Andersen R. A framework for the report of access to medical care. Wellness Serv Res. 1974;nine:208–20.
-
Raina P, O'Donnell M, Schwellnus H, et al. Caregiving procedure and caregiver brunt: conceptual models to guide enquiry and practice. BMC Pediatr. 2004;4:1.
-
Drotar D, Hack M, Taylor Chiliad, Schluchter Yard, Andreias L, Klein N. The touch on of extremely low nascency weight on the families of school-aged children. Pediatrics. 2006;117:2006–xiii.
-
Jessop DJ, Stein RE. Uncertainty and its relation to the psychological and social correlates of chronic illness in children. Soc Sci Med. 1985;20:993–9.
-
Stein RE, Jessop DJ. What diagnosis does not tell: the example for a noncategorical approach to chronic illness in childhood. Soc Sci Med. 1989;29:769–78.
-
Stein RE, Jessop DJ. Measuring health variables amongst Hispanic and non-Hispanic children with chronic weather condition. Public Wellness Rep. 1989;104:377–84.
-
Stein RE, Jessop DJ. The touch on on family scale revisited: further psychometric data. J Dev Behav Pediatr. 2003;24:9–16.
-
Landgraf JM, Vogel I, Oostenbrink R, van Baar ME, Raat H. Parent-reported health outcomes in infants/toddlers: measurement properties and clinical validity of the ITQOL-SF47. Qual Life Res. 2013;22:635–46.
-
Kruizinga I, Jansen W, van Sprang NC, Carter AS, Raat H. The Effectiveness of the BITSEA equally a Tool to Early Detect Psychosocial Problems in Toddlers, a Cluster Randomized Trial. PLoS 1. 2015;10:e0136488.
-
Flink IJ, Beirens TM, Looman C, et al. Wellness-related quality of life of infants from ethnic minority groups: the Generation R Study. Qual Life Res. 2013;22:653–64.
-
Flink IJ, Prins RG, Mackenbach JJ, et al. Neighborhood ethnic multifariousness and behavioral and emotional problems in 3 year olds: results from the Generation R Report. PLoS 1. 2013;8:e70070.
-
Raat H, Landgraf JM, Oostenbrink R, Moll HA, Essink-Bot ML. Reliability and validity of the Babe and Toddler Quality of Life Questionnaire (ITQOL) in a full general population and respiratory illness sample. Qual Life Res. 2007;16:445–threescore.
-
Oostenbrink R, Jongman H, Landgraf JM, Raat H, Moll HA. Functional abdominal complaints in pre-school children: parental reports of health-related quality of life. Qual Life Res. 2010;xix:363–9.
-
van Baar ME, Essink-Bot ML, Oen IM, et al. Reliability and validity of the Health Outcomes Burn Questionnaire for infants and children in The Netherlands. Burns. 2006;32:357–65.
-
ITQOL: Infant Toddler Quality of Life Questionnaire. (Accessed December 2nd, 2016, at healthactchq.com.)
-
Meert KL, Slomine BS, Christensen JR, et al. Family unit Burden Later on Out-of-Hospital Cardiac Abort in Children. Pediatr Crit Care Med. 2016;17:498–507.
-
van Zellem L, Buysse C, Madderom Chiliad, et al. Long-term neuropsychological outcomes in children and adolescents afterward cardiac arrest. Intensive Care Med. 2015;41:1057–66.
-
Rolfsjord LB, Skjerven HO, Carlsen KH, et al. The severity of astute bronchiolitis in infants was associated with quality of life nine months later. Acta Paediatr. 2016;105:834–41.
-
Doty M, Rustgi SD, Schoen C, Collins SR. Maintaining health insurance during a recession: probable COBRA eligibility: an updated analysis using the Commonwealth Fund 2007 Biennial Health Insurance Survey. Consequence brief. 2009;49:1–12.
-
Doty MM, Collins SR, Nicholson JL, Rustgi SD. Failure to protect: why the individual insurance market is not a viable option for most U.Southward. families: findings from the Commonwealth Fund Biennial Health Insurance Survey. Upshot brief. 2009;62:i–16.
-
Doty MM, Collins SR, Rustgi SD, Nicholson JL. Out of options: why so many workers in small businesses lack affordable health insurance, and how health care reform can help. Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2007. Outcome brief. 2009;67:1–22.
-
Rustgi SD, Doty MM, Collins SR. Women at risk: why many women are forgoing needed health care. An analysis of the Commonwealth Fund 2007 Biennial Health Insurance Survey. Event brief. 2009;52:i–12.
-
Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff Due south. Families' health-related social bug and missed referral opportunities. Pediatrics. 2007;119:e1332–41.
-
Hassan A, Blood E, Pikcilingis A, Krull E, McNickles L, Marmon K, Woods Due east, Fleegler E. Improving Social Determinants of Health: Effectiveness of a spider web-based intervention. Am J Prev Med. 2015;49(6):822-31. doi:10.1016/j.amepre.2015.04.023.
-
Hassan A, Blood EA, Pikcilingis A, et al. Youths' health-related social issues: concerns oftentimes overlooked during the medical visit. J Adolesc Health. 2013;53:265–71.
-
Wylie SA, Hassan A, Krull EG, et al. Assessing and referring adolescents' health-related social problems: qualitative evaluation of a novel web-based approach. J Telemed Telecare. 2012;xviii:392–8.
-
Statistics NCoH. National Health Interview Survey. Washington DC: Services UDoHaH, ed.; 1995.
-
Bureau UC. The American Housing Survey. Washington DC: Development DoHaU, ed; 1994.
-
Cress JFJ. The Philadelphia Survey of Kid Care and Work. Philadelphia, PA: Temple Academy; 2003.
-
Weinreb Fifty, Wehler C, Perloff J, et al. Hunger: its impact on children's health and mental health. Pediatrics. 2002;110:e41.
-
Accountable Health Communities Model. 2016. https://innovation.cms.gov/initiatives/AHCM). Accessed xviii December 2016.
-
Hediger ML, Overpeck Physician, Ruan WJ, Troendle JF. Birthweight and gestational age effects on motor and social evolution. Paediatr Perinat Epidemiol. 2002;16:33–46.
-
at http://www.nlsinfo.org/childya/nlsdocs/questionnaires/2006/Child2006quex/ MotherSupplement2006_Assessments.html#MOTORANDSOCIALDEVELOPMENT).
-
Belfort MB, Santo Eastward, McCormick MC. Using parent questionnaires to assess neurodevelopment in former preterm infants: a validation study. Paediatr Perinat Epidemiol. 2013;27:199–207.
-
Rivers A, Caron B, Hack M. Experience of families with very low birthweight children with neurologic sequelae. Clin Pediatr. 1987;26:223–30.
-
Taylor HG, Klein North, Minich NM, Hack 1000. Long-term family unit outcomes for children with very low birth weights. Arch Pediatr Adolesc Med. 2001;155:155–61.
-
Saigal S, Burrows Eastward, Stoskopf BL, Rosenbaum PL, Streiner D. Impact of extreme prematurity on families of adolescent children. J Pediatr. 2000;137:701–6.
-
Hodek JM, von der Schulenburg JM, Mittendorf T. Measuring economic consequences of preterm birth - Methodological recommendations for the evaluation of personal burden on children and their caregivers. Heal Econ Rev. 2011;1:6.
-
Petrou S. Economic consequences of preterm birth and low birthweight. BJOG. 2003;110 Suppl xx:17–23.
-
McCormick MC, Bernbaum JC, Eisenberg JM, Kustra SL, Finnegan E. Costs incurred by parents of very low nascence weight infants later on the initial neonatal hospitalization. Pediatrics. 1991;88:533–41.
-
Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol. 2007;27:614–ix.
-
Schiffman JK, Dukhovny D, Mowitz M, Kirpalani H, Mao Due west, Roberts R, Nyberg A, Zupancic J. Quantifying the Economic Burden of Neonatal Illness on Families of Preterm Infants in the U.Southward. and Canada. San Diego, CA: Pediatric Academic Societies; 2015.
-
Krieger J, Higgins DL. Housing and wellness: time again for public health action. Am J Public Wellness. 2002;92:758–68.
-
Rodgers JT, Purnell JQ. Healthcare navigation service in two-1-i San Diego: guiding individuals to the care they need. Am J Prev Med. 2012;43:S450–vi.
-
Jackson Grand, Ternestedt BM, Schollin J. From alienation to familiarity: experiences of mothers and fathers of preterm infants. J Adv Nurs. 2003;43:120–9.
-
Meijssen DE, Wolf MJ, Koldewijn K, van Wassenaer AG, Kok JH, van Baar AL. Parenting stress in mothers after very preterm nativity and the event of the Infant Behavioural Assessment and Intervention Program. Child Intendance Wellness Dev. 2011;37:195–202.
-
Melnyk BM, Oswalt KL, Sidora-Arcoleo K. Validation and psychometric properties of the neonatal intensive care unit parental beliefs scale. Nurs Res. 2014;63:105–xv.
-
Melnyk BM, Alpert-Gillis LJ. The COPE plan: a strategy to improve outcomes of critically ill young children and their parents. Pediatr Nurs. 1998;24:521–7.
-
Benzies KM, Magill-Evans JE, Hayden KA, Ballantyne M. Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13 Suppl i:S10.
-
Pighini MJ, Goelman H, Buchanan M, Schonert-Reichl Yard, Brynelsen D. Learning from parents' stories most what works in early on intervention. Int J Psychol. 2014;49:263–lxx.
-
Arockiasamy V, Holsti L, Albersheim South. Fathers' experiences in the neonatal intensive care unit: a search for control. Pediatrics. 2008;121:e215–22.
-
Phillips KA, Morrison KR, Anderson R, Aday LA. Agreement the context of healthcare utilization: Assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–96.
Acknowledgments
This study was supported by the Richardson Fund, Section of Neonatology, Beth Israel Deaconess Medical Centre, Boston MA, the Program for Patient Safety and Quality (PPSQ) at Boston Children's Infirmary, Boston, MA and the Medical Staff Organization at Boston Children's Hospital, Boston, MA.
We would like to thank the families who participated in this study. We would besides like to recognize Jane Stewart, Md, the managing director of the Babe Follow Upwards Plan (IFUP) at Boston Children's Hospital, Larry Rhein, MD, the manager of the Middle for Healthy Babe Lung Development (CHILD) program at Boston Children's Hospital and Janet Soul, MD, the director of the Fetal Neurology Program at Boston Children's Hospital who facilitated our study. We would also similar thank Brooke Corder, the social worker at the IFUP who assisted with patient recruitment. We would also like to acknowledge Aaron Picklingis who developed the spider web-interface for the report questionnaire and Drs. Dionne Graham and Sheree Schrager who assisted with statistical assay.
Funding
This study was also supported by the Richardson Fund with the Section of Neonatology, Beth Israel Deaconess Medical Center, Boston MA, the Program for Patient Safety and Quality (PPSQ) at Boston Children'southward Hospital, Boston, MA and the Medical Staff Organisation at Boston Children's Hospital, Boston, MA.
Availability of data and materials
The datasets generated during and/or analyzed during the current written report are not publicly bachelor due to patient information, but are bachelor from the corresponding author on reasonable asking.
Authors' contributions
Dr. Lakshmanan and Dr. Belfort made substantial contributions to designing the study, analyzing the data, and interpreting the results. Dr. Lakshmanan wrote the start draft of the manuscript. Ms. Agni collected the data and contributed to data analysis and drafting of the manuscript. Drs. Lieu, Fleegler and McCormick made substantial contributions to designing the study, interpreting the results, and critically revising the manuscript. Drs. Kipke and Friedlich also assisted in interpreting the results and revising the manuscript. All authors read and approved the last version of the manuscript.
Consent for publication
Non applicable. At that place is no identifiable data in this study.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent
The Boston Children'due south Hospital and Children's Infirmary Los Angeles homo subjects committees approved the study protocol and participation consent was obtained from all subjects.
Financial disclosure
Dr. Lakshmanan is supported by National Eye for Advancing Translational Scientific discipline (NCATS) of the U.South. National Institutes of Health (KL2TR001854). Dr. Belfort was supported by National Institutes of Health K23DK83817. The remaining authors have indicated they have no financial relationships relevant to this article to disclose.
Writer data
Affiliations
Corresponding author
Additional files
Additional file i:
Presurvey information demographics. (Doctor 108 kb)
Boosted file 2: Table S1.
Description of measurement instruments for primary outcomes, modifiable determinants and predisposing characteristics (potential confounders). (DOC 55 kb)
Rights and permissions
Open up Access This article is distributed nether the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original writer(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Artistic Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/nothing/1.0/) applies to the data fabricated available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Cite this commodity
Lakshmanan, A., Agni, Yard., Lieu, T. et al. The bear on of preterm birth <37 weeks on parents and families: a cantankerous-sectional study in the 2 years subsequently belch from the neonatal intensive care unit. Health Qual Life Outcomes fifteen, 38 (2017). https://doi.org/10.1186/s12955-017-0602-three
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12955-017-0602-3
Keywords
- Touch on on family
- Impact on parents
- Prematurity
- Loftier-risk babe
- Post-discharge
Source: https://hqlo.biomedcentral.com/articles/10.1186/s12955-017-0602-3
0 Response to "Health Problems of Low Birth Weight Babies on Family and Society"
Post a Comment